Volume 34, Issue 240 (12-2024)
J Mazandaran Univ Med Sci 2024, 34(240): 56-67 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Sarebannezhad F, Omidi A, Zanjani Z, Ghasemzadeh Hoseini E, Gholizadeh N. The Effectiveness of Mindfulness-Based Stress Reduction Therapy on Disease signs and Symptoms and Psychological Distress in Women with Oral Lichen Planus. J Mazandaran Univ Med Sci 2024; 34 (240) :56-67
URL: http://jmums.mazums.ac.ir/article-1-21406-en.html
URL: http://jmums.mazums.ac.ir/article-1-21406-en.html
Fatemeh Sarebannezhad 
 , Abdollah Omidi
, Abdollah Omidi 
 , Zahra Zanjani
, Zahra Zanjani 
 , Elaheh Ghasemzadeh Hoseini
, Elaheh Ghasemzadeh Hoseini 
 , Narges Gholizadeh
, Narges Gholizadeh 


 , Abdollah Omidi
, Abdollah Omidi 
 , Zahra Zanjani
, Zahra Zanjani 
 , Elaheh Ghasemzadeh Hoseini
, Elaheh Ghasemzadeh Hoseini 
 , Narges Gholizadeh
, Narges Gholizadeh 

Abstract: (1550 Views)
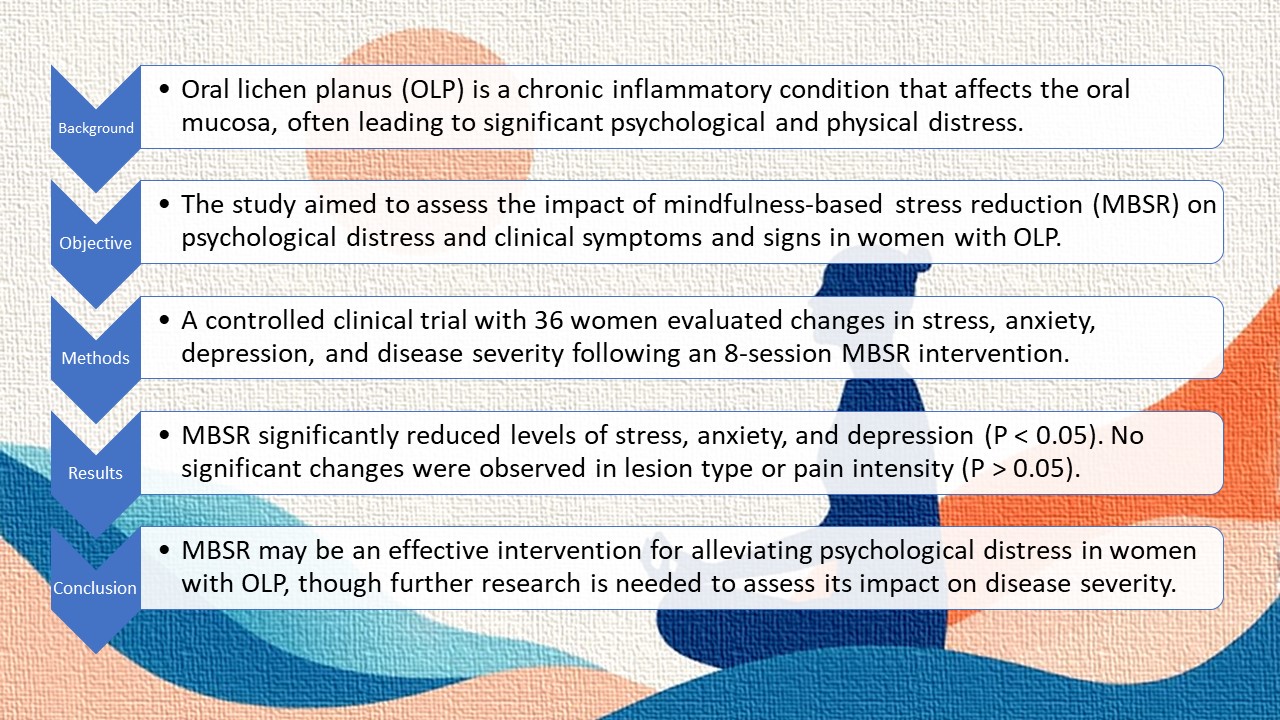
Background and purpose: Oral lichen planus (OLP) is a chronic inflammatory autoimmune disease that, although not typically life-threatening, can lead to significant psychosocial consequences. Due to its persistent nature and the lack of effective treatments to prevent its progression, OLP can severely impact quality of life. The aim of the present study is to investigate the effectiveness of mindfulness-based stress reduction therapy in alleviating symptoms and signs of the disease, as well as reducing stress, anxiety, and depression in women with oral lichen planus.
Materials and methods: This study is a controlled clinical trial with a pre-test/post-test design. The sample comprised 36 women diagnosed with oral lichen planus, who were selected using purposive sampling and were then randomly assigned to either the control or experimental group. Data were collected using the DASS-21 questionnaire, Visual Analog Scale (VAS), and Thongprasom Scale. The experimental group received 8 sessions of Mindfulness-Based Stress Reduction (MBSR) therapy, while the control group received no interventions. Data were analyzed using SPSS software (version 22).
Results: In the experimental group, the mean scores for stress, anxiety, and depression in the post-test phase were 9.29±4.22, 5.94±3.92, and 7.00±5.55, respectively. In the control group, these scores were 10.94±4.84, 7.71±4.70, and 9.65±5.44, respectively. After adjusting for pre-test scores, the results of covariance analysis showed that the mean scores of the experimental and control groups differed significantly for these variables in the post-test phase (P<0.05). The mean intensity of pain or burning sensation in the experimental group during the post-test phase was 2.94±1.85, compared to 3.65±1.69
in the control group; however, this difference was not statistically significant. Similarly, there was
no statistically significant difference in the frequency of lesions between the experimental and control groups (P>0.05).
Conclusion: The results of this study indicate that MBSR can be an effective approach to reducing psychological distress in patients with oral lichen planus.
(Clinical Trials Registry Number: IRCT20221204056709N1)
Materials and methods: This study is a controlled clinical trial with a pre-test/post-test design. The sample comprised 36 women diagnosed with oral lichen planus, who were selected using purposive sampling and were then randomly assigned to either the control or experimental group. Data were collected using the DASS-21 questionnaire, Visual Analog Scale (VAS), and Thongprasom Scale. The experimental group received 8 sessions of Mindfulness-Based Stress Reduction (MBSR) therapy, while the control group received no interventions. Data were analyzed using SPSS software (version 22).
Results: In the experimental group, the mean scores for stress, anxiety, and depression in the post-test phase were 9.29±4.22, 5.94±3.92, and 7.00±5.55, respectively. In the control group, these scores were 10.94±4.84, 7.71±4.70, and 9.65±5.44, respectively. After adjusting for pre-test scores, the results of covariance analysis showed that the mean scores of the experimental and control groups differed significantly for these variables in the post-test phase (P<0.05). The mean intensity of pain or burning sensation in the experimental group during the post-test phase was 2.94±1.85, compared to 3.65±1.69
in the control group; however, this difference was not statistically significant. Similarly, there was
no statistically significant difference in the frequency of lesions between the experimental and control groups (P>0.05).
Conclusion: The results of this study indicate that MBSR can be an effective approach to reducing psychological distress in patients with oral lichen planus.
(Clinical Trials Registry Number: IRCT20221204056709N1)
Keywords: Oral lichen planus, stress, anxiety, depression, pain, burning, mucosal lesions, mindfulness-based stress reduction
Type of Study: Research(Original) |
Subject:
psychology
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |