Volume 34, Issue 236 (8-2024)
J Mazandaran Univ Med Sci 2024, 34(236): 94-99 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Setareh J, Nejati Z, Masoudzadeh A, Nadi Ghara A. The Relationship between Sleep Disorders, Anxiety, and Depression with Obsessive-Compulsive Severity of Symptoms in Patients with OCD. J Mazandaran Univ Med Sci 2024; 34 (236) :94-99
URL: http://jmums.mazums.ac.ir/article-1-19700-en.html
URL: http://jmums.mazums.ac.ir/article-1-19700-en.html
Abstract: (2211 Views)
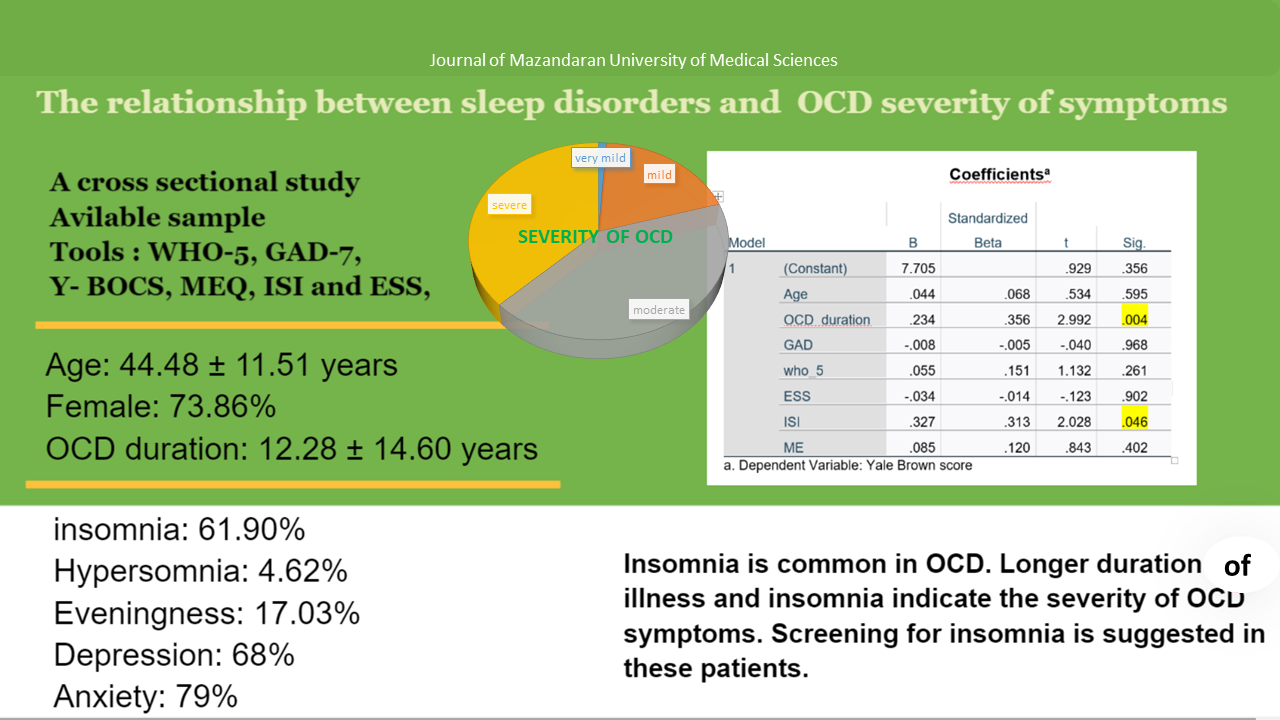
Background and purpose: Accompanying sleep disorders such as insomnia, delayed sleep, and wakefulness, as well as anxiety and depression with obsessive-compulsive disorder, are common in patients with OCD. However, not much research has been done on the relationship between sleep disorders and the severity of symptoms in patients with OCD. This article examines the frequency and relationship between sleep disorders, depression, anxiety, and the severity of obsessive-compulsive symptoms in patients with OCD.
Materials and methods: Convenience sampling was used in this cross-sectional research. The participants in the study were those who were referred to the clinic of a psychiatric hospital and the central clinic complex in Sari. Obsessive-compulsive disorder diagnosis of the participants was confirmed by a psychiatrist based on DSM-5 diagnostic criteria. Eighty-eight patients participated in the study after obtaining informed consent. Demographic questionnaires, Yale-Brown Obsessive-Compulsive Scale (Y-BOCS), morning-evening questionnaire (MEQ), Epworth Sleepiness Scale (ESS), Insomnia Severity Index (ISI), WHO-5 well-being (Depression) Index, and Generalized Anxiety Disorder-7 (GAD-7). Data analysis was done with SPSS version 20 software.
Results: Out of 88 patients, 65 (73.86%) were women 23 (26.14%) were men, 71.59% were married, 57.95% had under diploma degree, and 94.22% had no history of drug use. The average age of the patients was 44.48 ± 11.51 years. The duration of OCD was 11.28±14.60 years In terms of the severity of OCD symptoms, 1.1% was very mild, 19.32% was relatively mild, 42.45% was moderate, and 37.50% was severe. In the type of sleep schedule, 17.03% were inclined to evening or relative evening type. Four patients (4.62%) had daytime sleepiness. Also, 52 patients (61.90%) had some degree of insomnia. In terms of the severity of insomnia, 23.86% were mild, 28.40% were moderate and 6.81% were severe. The frequency of depression was 68% and anxiety was 79%. No statistically significant relationship was found between the severity of obsessive-compulsive disorder and hypersomnia, evening chronotype, anxiety, and depression. But insomnia (P= 0.046) and duration of illness (P= 0.004) were related to it. The Pearson correlation coefficient between age, duration of obsessive-compulsive disorder, and severity of obsessive-compulsive symptoms was 0.169 (P= 0.116) and 0.377 (P=0.001), respectively. Spearman's correlation coefficient between the severity of obsessive-compulsive symptoms with depression and anxiety was 0.090 (P=0.403) and 0.044 (P=0.685), respectively. The average severity of obsessive-compulsive symptoms was 23.48±7.87 in women and 20.04±5.88 in men, and no significant difference was seen in both sexes (P=0.060). In linear regression, the two factors affecting the severity of obsessive-compulsive symptoms were the duration of the illness and the severity of insomnia.
Conclusion: Considering the higher frequency of insomnia in patients with obsessive-compulsive disorder compared to the normal population and its role in the severity of obsessive-compulsive disorder symptoms, it is necessary to examine patients with obsessive-compulsive disorder in terms of insomnia. Also, older OCD patients should be examined more carefully in terms of the severity of obsessive-compulsive symptoms.
Materials and methods: Convenience sampling was used in this cross-sectional research. The participants in the study were those who were referred to the clinic of a psychiatric hospital and the central clinic complex in Sari. Obsessive-compulsive disorder diagnosis of the participants was confirmed by a psychiatrist based on DSM-5 diagnostic criteria. Eighty-eight patients participated in the study after obtaining informed consent. Demographic questionnaires, Yale-Brown Obsessive-Compulsive Scale (Y-BOCS), morning-evening questionnaire (MEQ), Epworth Sleepiness Scale (ESS), Insomnia Severity Index (ISI), WHO-5 well-being (Depression) Index, and Generalized Anxiety Disorder-7 (GAD-7). Data analysis was done with SPSS version 20 software.
Results: Out of 88 patients, 65 (73.86%) were women 23 (26.14%) were men, 71.59% were married, 57.95% had under diploma degree, and 94.22% had no history of drug use. The average age of the patients was 44.48 ± 11.51 years. The duration of OCD was 11.28±14.60 years In terms of the severity of OCD symptoms, 1.1% was very mild, 19.32% was relatively mild, 42.45% was moderate, and 37.50% was severe. In the type of sleep schedule, 17.03% were inclined to evening or relative evening type. Four patients (4.62%) had daytime sleepiness. Also, 52 patients (61.90%) had some degree of insomnia. In terms of the severity of insomnia, 23.86% were mild, 28.40% were moderate and 6.81% were severe. The frequency of depression was 68% and anxiety was 79%. No statistically significant relationship was found between the severity of obsessive-compulsive disorder and hypersomnia, evening chronotype, anxiety, and depression. But insomnia (P= 0.046) and duration of illness (P= 0.004) were related to it. The Pearson correlation coefficient between age, duration of obsessive-compulsive disorder, and severity of obsessive-compulsive symptoms was 0.169 (P= 0.116) and 0.377 (P=0.001), respectively. Spearman's correlation coefficient between the severity of obsessive-compulsive symptoms with depression and anxiety was 0.090 (P=0.403) and 0.044 (P=0.685), respectively. The average severity of obsessive-compulsive symptoms was 23.48±7.87 in women and 20.04±5.88 in men, and no significant difference was seen in both sexes (P=0.060). In linear regression, the two factors affecting the severity of obsessive-compulsive symptoms were the duration of the illness and the severity of insomnia.
Conclusion: Considering the higher frequency of insomnia in patients with obsessive-compulsive disorder compared to the normal population and its role in the severity of obsessive-compulsive disorder symptoms, it is necessary to examine patients with obsessive-compulsive disorder in terms of insomnia. Also, older OCD patients should be examined more carefully in terms of the severity of obsessive-compulsive symptoms.
Keywords: obsessive-compulsive disorder, hypersomnia, insomnia, delayed sleep-wake phase disorder, anxiety and depression
Type of Study: Brief Report |
Subject:
psychiatry
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |